News Summary
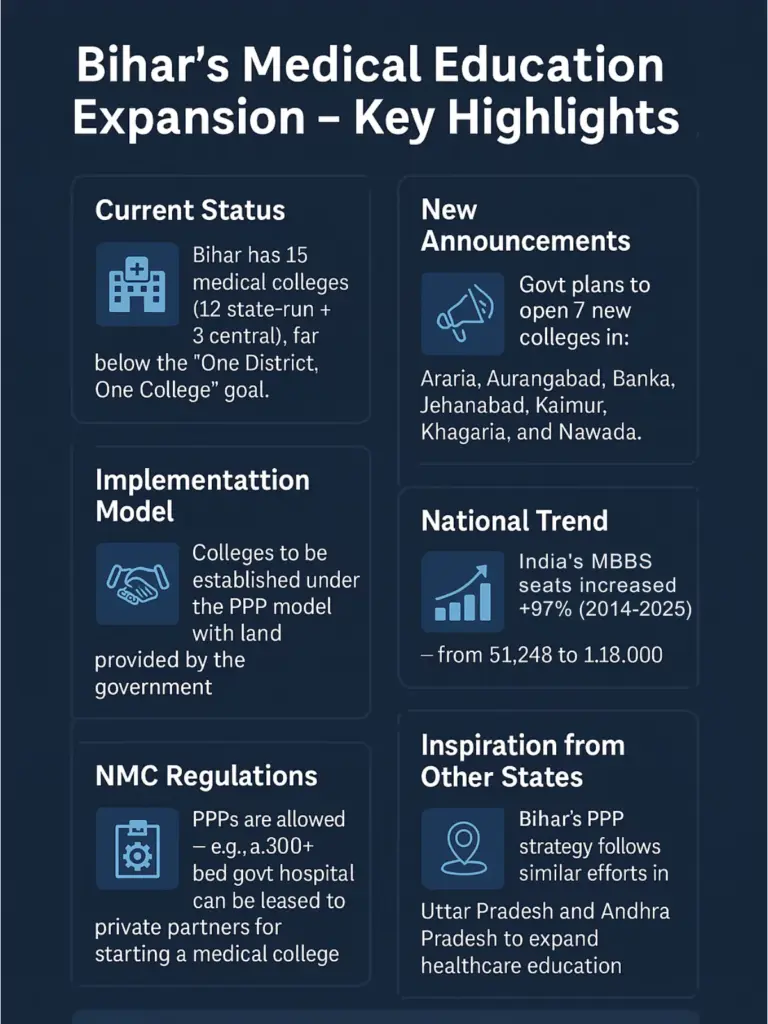
- Bihar has only 15 medical colleges (12 state-run plus 3 central institutions)
- The Govt to introduce the PPP model for rapid expansion
- The risk of social security erosion, free service, and high out-of-pocket costs looms
- Institutional and Public oversight is needed to mitigate risks
The Bihar government announced that it will invite private firms to run selected public medical colleges and hospitals under a public–private partnership (PPP) model. Under this plan, the state will provide land and part of the capital cost for new medical colleges and hospitals, while private partners will fund and manage construction and operations.
Deputy Chief Minister Samrat Chowdhary made these remarks on Friday while addressing the inaugural ceremony of the two-day Health Fair held at Gyan Bhawan in Patna. Meanwhile, the Health Minister Mangal Pandey claimed that Bihar’s healthcare services have transformed significantly over the past 20 years.
This initiative, part of the state’s goal to have at least one medical college in each of its 38 districts, represents a major shift in Bihar’s health policy.
To understand its implications, we examine the potential benefits and drawbacks of PPPs for Bihar’s medical education and healthcare, drawing on data and experience from India’s health sector.
PPP Model for Medical Colleges: Potential Benefits
- Capacity Expansion: Private involvement can accelerate the pace of medical infrastructure development. With limited public funding, PPPs can ensure rapid creation of new medical colleges and thousands of new MBBS seats.
- Modern Infrastructure and Technology: Private entities often bring modern technology and equipment. An example is the IFC-supported PPP in Jharkhand, which upgraded diagnostics in 24 hospitals. Gujarat’s GAIMS hospital, a successful PPP, serves as a benchmark with its 750-bed modern facility.
- Expertise and Efficiency: Private healthcare accounts for over 80% of India’s doctors. Through PPPs, Bihar can tap into this talent, implementing digital health records, modern teaching methodologies, and efficient management systems.
- Financial Sustainability: By sharing construction and operational costs, PPPs reduce the financial burden on the state. Schemes like Viability Gap Funding allow states to stretch their limited budgets further.
- Employment Generation More colleges mean more jobs, not just for doctors and faculty but for nurses, technicians, and administrative staff. PPPs can also help fill teaching vacancies that have plagued Bihar and other states.
In sum, potential benefits include rapidly increasing the number of doctors and health facilities, improving infrastructure, leveraging private know-how, and easing state budgets.
These benefits are especially attractive in Bihar, where per-capita health spending is low and public hospitals are overcrowded.
The example of GAIMS shows that a long-term PPP can deliver a modern teaching hospital where none existed.
PPP Model for Medical Colleges: Potential Drawbacks
However, experts also warn of significant risks and challenges with PPPs in healthcare. Key concerns include:
- Affordability and Cost Inflation: Private facilities generally charge higher fees. There’s a risk that poor patients will lose access to free services or be pushed toward insurance-based schemes like Ayushman Bharat.
- Equity Concerns: Studies show that private healthcare often caters to higher-income patients. If not carefully regulated, PPP colleges may prioritise profit over inclusivity.
- Quality and Oversight: Profit motives may compromise care quality. Bihar’s own PPP diagnostic labs faced scrutiny for poor service standards. Weak monitoring could allow private partners to neglect their obligations.
- Impact on the Public Sector: Handing over district hospitals to private players could sideline public sector staff, leading to job insecurity and morale issues. Contract workers often face worse pay and conditions.
- Political and Social Resistance: Public healthcare privatisation has faced backlash in states like Tamil Nadu and Madhya Pradesh. Bihar must build public trust through transparency and strong grievance redressal mechanisms.
In summary, potential downsides include higher out-of-pocket costs for patients, erosion of free services, quality and equity risks, and weakened public capabilities.
These are not theoretical: past PPP attempts in health (e.g. Karnataka’s Apollo and NGO experiments) have failed and been unwound.
Thus, Bihar must tread carefully and ensure strict contract enforcement (e.g. for reserved beds), transparent monitoring, and mechanisms to protect the poor.
Comparative Analysis
Evidence from other states highlights both the benefits and drawbacks of PPP in medical education. Gujarat’s GAIMS (the Adani partnership) is a noted success: it has created a modern teaching hospital in rural Kutch with all classes of patients, funded largely by private capital.
Bihar could replicate this model to build centers of excellence.
Uttar Pradesh’s rapid college expansion (now 64 districts covered) has been achieved with a mix of government and private colleges; the state reports that new medical institutions not only improve care but also generate local jobs.
On the other hand, lessons from failures must inform Bihar’s approach. The Karnataka experience shows that without vigilant oversight, private operators may underperform; indeed, its first PPP hospital had to be taken back by the government after unmet obligations.
The Oxfam study urges that PPP services should supplement, not substitute, public health infrastructure.
Bihar’s own past PPP in diagnostics increased access but also led to idle public labs, hinting that outsourcing entire functions can inadvertently weaken the system.
Any PPP rollout in Bihar will also face the state’s specific challenges: severe doctor and staff shortages, especially in rural areas. If private partners cannot find or afford to recruit enough qualified teachers, new colleges may open in name only.
Other states have cited faculty vacancies as a motivator for PPP, but PPPs do not automatically solve the problem of attracting doctors to remote postings. Bihar must ensure that PPP agreements include commitments to recruit and retain quality faculty and to offer affordable seats.
For Bihar, the success of this policy will hinge on implementation details. The government must safeguard affordability (for example, strictly enforce reserved free beds) and protect quality (through ongoing audits and penalties for non-compliance).
It should leverage PPP advantages, technology, efficiency and funding, while maintaining a robust public sector backbone. With vigilant oversight and a clear focus on public health goals, Bihar’s PPP experiment could help train more doctors and improve care; without it, there is a risk of simply shifting public assets into private hands without lasting public benefit