India, with over 700 medical colleges, has the world’s largest number of medical colleges. In comparison, China has fewer than 200 medical colleges. Despite this, China produces more doctors annually than India. This anomaly raises urgent questions about the effectiveness of India’s medical education system and what reforms are necessary to address the nation’s growing healthcare needs.
The Numbers Game
- China: Roughly 140,000 new doctors graduate every year.
- India: Despite rapid expansion, only about 780 medical colleges and 110,000 MBBS seats exist as of 2025, with actual yearly graduates slightly lower due to dropouts and delayed completions.
- As of 2024, China has over 180 medical colleges and universities that are officially recognised to offer medical education programs.
While the numbers seem close, China’s production is more consistent, better distributed, and supported by a more robust public healthcare network. Importantly, China manages this with fewer institutions, indicating superior institutional efficiency.
Key Reasons Why China Produces More Doctors Than India
1. Larger Batch Sizes and Uniform Distribution
China’s medical colleges admit significantly larger batches per institution, often 800-1200 students annually, compared to India’s average of 150-250 per college. This is due to:
- Better hospital-to-seat ratios.
- Centralised health infrastructure planning.
- Larger teaching hospitals with integrated training.
2. Integrated Public Health and Medical Education
In China, public hospitals are directly linked with medical universities, ensuring seamless clinical training, internships, and placements. India’s medical colleges, especially in the private sector, often suffer from:
- Inadequate clinical exposure.
- Hospital attachments without real patient flow.
- Faculty shortages.
3. Low-Cost Public Education
Most of China’s medical education is state-funded, making it accessible to a broader section of students. India’s overdependence on private medical education, where fees often exceed ₹60–80 lakh, limits the number of students who can afford to complete MBBS.
4. Streamlined Admissions and Standard Curriculum
- China follows a centralised entrance and placement system governed by the Ministry of Education and Health.
- India’s system is fragmented: multiple counselling rounds, quota battles, and legal stays create inefficiencies.
- China’s curriculum is standardised nationally, focusing on preventive, primary, and rural healthcare, unlike India’s largely tertiary-care, urban-focused education.
5. Robust Use of Traditional and Allied Medicine
China has integrated Traditional Chinese Medicine (TCM) into its national health system. This has:
- Expanded the number of trained health professionals.
- Reduced the dependency on allopathic doctors for minor illnesses.
India, despite its AYUSH sector, has failed to mainstream it effectively within rural and primary health services.
Important Points to Note:
China leads as the source of MBBS graduates in India: Between 2012–2014, 11,825 Indian students with Chinese MBBS degrees took India’s FMGE screening exam, more than those from Russia (5,950) and Nepal (3,163)
Cost and accessibility drivers: Countries like China and Nepal attract students due to lower tuition fees than private institutions in India and less costly than European options.
What India Can Learn from China’s Model
1. Focus on Quality Over Quantity in Medical Colleges
India’s rapid expansion of private medical colleges has not been matched with infrastructure, faculty, or hospital quality. Lessons:
- Strengthen existing institutions before licensing new ones.
- Enforce strict quality control and teacher-student ratios.
2. Revamp Public Sector Medical Education
- Increase MBBS seats in government colleges instead of relying on private players.
- Offer tuition waivers or scholarships to students willing to serve in rural areas, similar to China’s rural service model.
3. Better Integration of Health Services and Education
- Link all medical colleges mandatorily with district hospitals and Community Health Centres (CHCs).
- Encourage primary-care-based training, not just super-speciality exposure.
4. Expand Batch Sizes Where Feasible
- In India, most government colleges can safely double batch sizes if infrastructure is upgraded.
- Faculty augmentation and digital learning platforms (e.g., NMC’s e-resources) should be used to scale education safely.
5. Digitise and Simplify NEET Counselling
- Learning from China’s streamlined admission process, India must reform NEET UG counselling by:
- Eliminating opaque quotas.
- Ensuring one centralised system for both private and government seats.
6. Leverage AYUSH and Mid-Level Healthcare Workers
- Formalise training and integration of mid-level healthcare providers, such as Community Health Officers (CHOs).
- Promote AYUSH practitioners as part of preventive healthcare teams, especially in underserved regions.
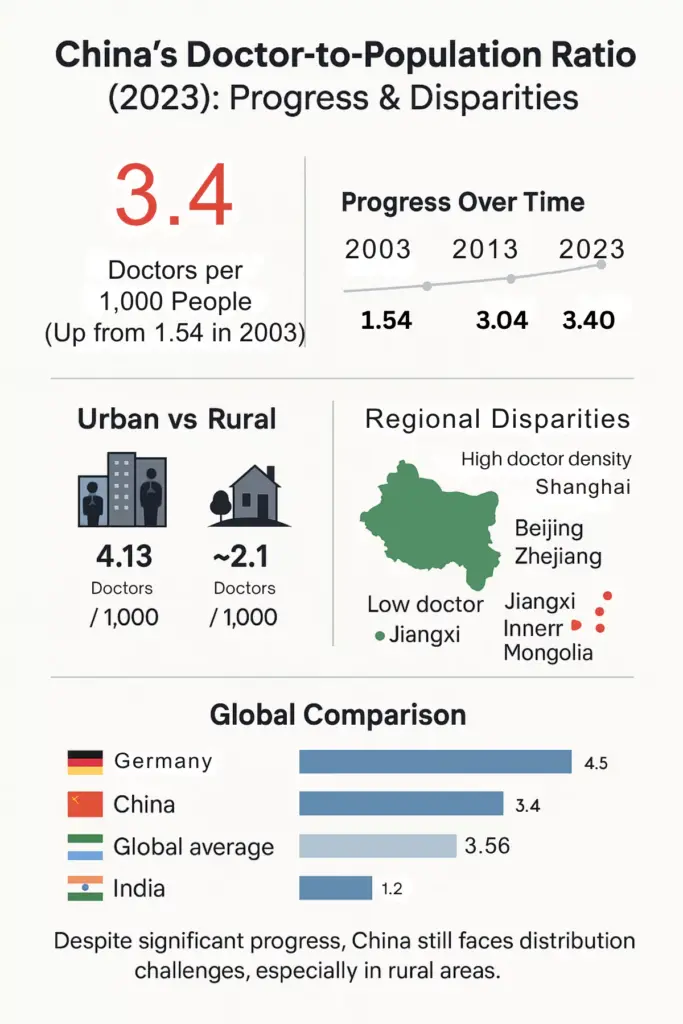
India’s healthcare demands are exploding, yet the doctor-population ratio remains poor due to inefficiencies in medical education. China’s ability to produce more doctors with fewer colleges is a clear sign of a well-optimised, state-backed system that India can learn from.
If India aspires to achieve universal healthcare, it must stop focusing merely on increasing MBBS seats and instead reform the system holistically, from college infrastructure and public sector investment to rural service mandates and curriculum overhaul.
India doesn’t need more medical colleges; it needs better ones, stronger systems, and a clear national vision to train the doctors of tomorrow.