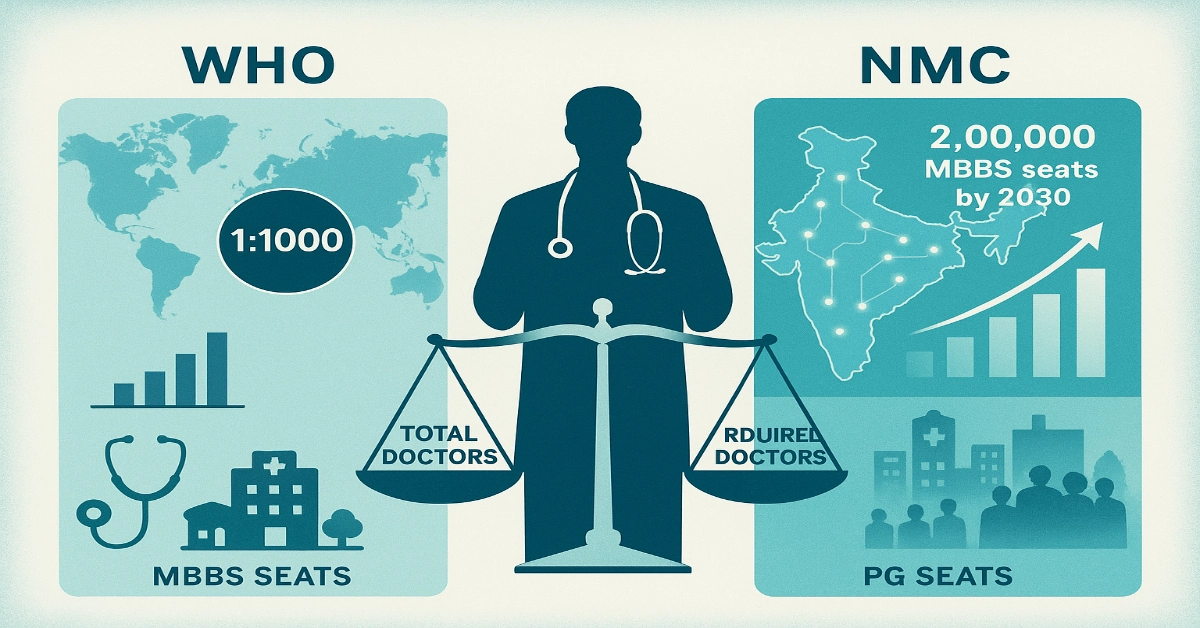
WHO vs NMC Projection Model: India is expanding medical education at a record pace. With over 800 medical colleges and more than 1.3 lakh MBBS seats, the National Medical Commission (NMC) and the Union Government are rapidly increasing the country’s doctor-production capacity. Yet one foundational question continues to dominate policy-making and public debate:
How many doctors does India actually need by the year 2030?
Is the current expansion enough? Or is the country still far short of global benchmarks?
To answer this, we construct a WHO vs NMC Projection Model, estimate the ideal doctor-population ratio, calculate the required number of PG specialists, and analyse state-wise and rural-urban distribution gaps.
This article analyse what India must achieve before 2030 to build an equitable and efficient healthcare system.
The WHO Benchmark: How Many Doctors Should India Ideally Have?
The World Health Organization (WHO) recommends a minimum doctor-population ratio of 1:1000 for any functional healthcare system.
India currently has an approximate ratio of 1:1300, only accounting for allopathic doctors.
To meet WHO standards by 2030, we roughly take India’s population of 150 crore.
WHO Requirement Calculation
- Required doctors = 15 lakh
- Estimated currently active doctors = 14 Lakh (13,86,150) registered allopathic doctor
- Assume that 80% of registered practitioners are available
- Practicing doctors = 11.2 Lakh
- Shortfall = approx. 4 lakh doctors
This suggests that India must add at least 4 lakh more practising doctors to meet global adequacy.
However, this is only the national number. The distribution of doctors, and the availability of specialists, is where India’s real crisis lies.
The NMC Projection Model: How Many Doctors Will India Produce by 2030?
The National Medical Commission is approving:
- New medical colleges
- Seat increases in existing colleges
- Conversion of district hospitals into teaching college
If this speed continues, India’s MBBS seat is expected to touch 2 lakh seats per year by 2030.
As the PM Modi through a cabinet decision ordered to add 75 thousands medical seats across India over next five years. Recently the Union Cabinet approved 5000 PG & 5023 MBBS Seats under Phase III of Central sector Scheme for Medical College expansion plan.
Projected Output 2025-2030
- Total new MBBS doctors added: 7.5-8 lakh
- After accounting for dropouts and non-clinical career shifts: 6-6.5 lakh active practising doctors
Total doctors by 2030
- Existing base: around 11 lakh
- New entrants (net): 6-6.5 lakh
Total: approx. 17-17.5 lakh doctors
This number exceeds WHO’s requirement on paper.
But the NMC model also highlights major structural challenges:
- Specialist shortages
- Extreme rural-urban divide
- State-level differences
- Understaffed district hospitals
- Weak retention in backward regions
India may meet WHO norms in total numbers but still fail to achieve equitable healthcare accessibility.
The Distribution Problem: Why India’s Real Shortage Is Rural
More than 65% of India’s population lives in rural areas, but less than 25% of doctors practise there.
Even with the projected increase in the number of doctors by 2030, the inequality in their distribution remains enormous.
Urban areas are expected to have a doctor density of roughly 1:600-700, while rural regions may remain at a much weaker ratio of 1:2000-2500, significantly worse than the WHO’s recommended standard.
This inequality is driven by a multiple structural issues. The rural PHCs and CHCs mostly lack adequate infrastructure, district hospitals struggle to offer specialty services, and essential diagnostic or emergency equipment is frequently missing.
At the same time, doctors posted in remote areas face poor living conditions, limited postgraduate training opportunities, and salaries that fail to compete with urban or private-sector roles.
Inconsistencies in state-level policies further discourage long-term retention. As a result, India’s projected doctor surplus on paper hides a much deeper and more persistent distribution crisis.
State-Wise Doctor Shortage Forecast for 2030
India’s medical landscape is highly uneven. Some states already have strong doctor density and surplus medical colleges, while others lag far behind.
States likely to be well-positioned by 2030
- Tamil Nadu
- Kerala
- Karnataka
- Andhra Pradesh
- Delhi
- Puducherry
These regions benefit from:
- Higher MBBS and PG seat density
- Better retention
- Strong infrastructure
- Mature private healthcare markets
States expected to remain critically short
- Uttar Pradesh
- Bihar
- Jharkhand
- Madhya Pradesh
- Rajasthan
- Odisha
- Chhattisgarh
- Most Northeast states (except Assam)
The challenges here include:
- High population base
- Lower medical college presence
- Fewer PG seats
- Poor district hospital infrastructure
- Difficulty retaining doctors
- Weak private healthcare growth
India’s doctor shortage is fundamentally a state-level crisis, not just a national one.
The Specialist Crisis: Why India Needs 5 Lakh More PG Seats
While India is rapidly expanding its MBBS capacity, the country’s postgraduate ecosystem is not keeping pace. At present, India produces around 1.30 lakh MBBS graduates every year, but offers only about 70,000-80,000 PG seats across MD, MS, and DNB programmes.
In simple terms, only 55-60 postgraduate seats exist for every 100 MBBS seats, a mismatch that creates a bottleneck in the medical education pipeline. Ideally, a balanced healthcare system requires a 1:1 ratio of MBBS to PG seats, ensuring that every medical graduate gets a fair chance to specialise.
To meet India’s growing healthcare needs, the country will have to add at least 70,000-80,000 new PG seats by 2030. Otherwise, specialist shortages will remain severe in critical disciplines such as anaesthesia, radiology, general medicine, cardiology, critical care, surgery, and other superspecialty fields.
District hospitals and public health facilities will continue to face specialist vacancies, even if the overall number of MBBS graduates rises sharply. India is increasing the quantity of doctors, but without parallel growth in specialist training, the healthcare system’s backbone will continue to stay weak.
Why Expanding MBBS Seats Won’t Fix Healthcare
Rapid MBBS expansion only addresses the basic shortage of doctors, but it does not tackle the deeper structural issues.
- Specialist scarcity continues because MBBS graduates cannot fill critical posts in anaesthesia, radiology, emergency care, or surgery.
- Rural infrastructure remains weak, with many PHCs and CHCs lacking diagnostics, ICUs, or functioning labs, making it impossible for doctors to deliver quality care.
- Regional imbalances exist, as southern states move toward surplus while northern and eastern states continue to face severe deficits.
- At the same time, migration patterns drain capacity, with doctors shifting from rural to urban areas, from government to private hospitals, and eventually overseas in search of better pay and working conditions.
- Finally, PG faculty shortages limit specialist training, slowing the expansion of MD/MS seats. In short, India needs a full healthcare ecosystem upgrade, not just more medical colleges.
Read Also: WHO vs NMC Projection Model, How Many Doctors India Needs in 2030
Policy Roadmap: What India Must Do Before 2030
A multi-dimensional approach is required to balance doctor production, distribution, and specialization.
Expand PG Seats Substantially
- Add 70,000-80,000 seats
- Strengthen DNB capacity
- Encourage private hospitals to start PG programs
- Upgrade district hospitals to PG teaching centres
Rebuild Rural Health Infrastructure
- Expand CHCs into 200-bed specialty centres
- Add ICUs, CT/MRI, trauma care units
- Improve ambulance networks
- Strengthen telemedicine and AI-based diagnostics
Introduce Better Rural Service Incentives
- Higher rural salaries
- PG admission advantages
- Housing and transport facilities
- Loan repayment schemes
Fix State-Level Disparities
- Prioritise underserved states for seat expansion
- Ensure retention policies for doctors
- Introduce special incentives for backward regions
Improve Working Conditions
- Timely stipends
- Safer workplaces
- Regulated working hours
- Strong mentorship and academic support
What Happens If India Misses the 2030 Targets?
Failure to correct the distribution and specialization gaps will lead to:
- Persistent rural mortality
- Overcrowded urban hospitals
- Intensifying PG competition
- Unstaffed district hospital specialties
- Costlier private healthcare
- Higher doctor migration
- More NEXT exam failures due to poor clinical exposure
India risks having enough MBBS doctors but an ineffective healthcare system.
By 2030, India will likely produce enough MBBS doctors to meet the WHO’s benchmark. However, the real challenges lie elsewhere:
- Unequal distribution across states
- A weak rural healthcare ecosystem
- A severe shortage of specialists
- Limited PG seats
- Low retention in underserved regions
To ensure meaningful healthcare access for its 150 crore citizens, India must:
- Expand PG seats
- Strengthen rural hospitals
- Improve working conditions
- Balance state-level inequities
Only a comprehensive and equitable strategy can transform India’s rapid doctor-production boom into improved healthcare outcomes.